Cystic fibrosis pseudomonas is a critical concern for individuals living with cystic fibrosis, as the bacteria Pseudomonas aeruginosa is one of the most common pathogens affecting their respiratory systems. This persistent infection can lead to chronic lung damage, making it a major contributor to the decline in lung function experienced by cystic fibrosis patients. Understanding how this bacteria interacts with the body, its impact on health, and the available treatment options is crucial for managing the disease effectively. With advancements in medical research and personalized care, there is hope for improved outcomes and quality of life for those affected.
Pseudomonas aeruginosa thrives in the thick mucus that accumulates in the lungs of cystic fibrosis patients, creating an environment where it can establish chronic infections. These infections are notoriously difficult to treat due to the bacteria's resistance to antibiotics and its ability to adapt to the host's immune system. This resistance often leads to prolonged treatment regimens and the need for innovative therapies. By exploring the relationship between cystic fibrosis and pseudomonas, patients and healthcare providers can better anticipate challenges and develop strategies to combat this persistent threat.
Living with cystic fibrosis pseudomonas requires a multidisciplinary approach, combining medical interventions, lifestyle adjustments, and emotional support. Patients must work closely with their healthcare team to monitor symptoms, manage flare-ups, and prevent further complications. Early detection and proactive management are key to minimizing the impact of pseudomonas infections and maintaining lung health. With the right resources and guidance, individuals with cystic fibrosis can navigate the complexities of pseudomonas-related issues and lead fulfilling lives.
Read also:Unraveling The Mystery Behind The Crash At Bristol
Table of Contents
- What is Cystic Fibrosis Pseudomonas?
- How Does Pseudomonas Affect Cystic Fibrosis Patients?
- What Are the Symptoms of Pseudomonas Infections?
- Why Is Pseudomonas Difficult to Treat in Cystic Fibrosis?
- How Can Pseudomonas Infections Be Prevented?
- Current Treatment Options for Cystic Fibrosis Pseudomonas
- Emerging Therapies on the Horizon
- What Role Does Genetics Play in Cystic Fibrosis?
- How Can Patients Manage Their Condition Effectively?
- Frequently Asked Questions About Cystic Fibrosis Pseudomonas
What is Cystic Fibrosis Pseudomonas?
Cystic fibrosis pseudomonas refers to the presence of Pseudomonas aeruginosa bacteria in individuals with cystic fibrosis. This gram-negative bacterium is particularly problematic for cystic fibrosis patients due to its ability to thrive in the thick, sticky mucus that accumulates in their lungs. Once established, pseudomonas infections can lead to chronic respiratory issues, making it a significant contributor to morbidity in this population.
How Does Pseudomonas Affect Cystic Fibrosis Patients?
Pseudomonas aeruginosa is highly adaptable and can form biofilms, which are protective layers that shield the bacteria from the immune system and antibiotics. These biofilms make it difficult to eradicate the infection, leading to persistent lung damage over time. The bacteria also release toxins that further inflame the airways, exacerbating the symptoms of cystic fibrosis.
What Are the Symptoms of Pseudomonas Infections?
Common symptoms of pseudomonas infections in cystic fibrosis patients include increased coughing, production of green or yellow mucus, shortness of breath, and fatigue. These symptoms often worsen during flare-ups, which can significantly impact the patient's quality of life. Early recognition of these signs is crucial for timely intervention.
Why Is Pseudomonas Difficult to Treat in Cystic Fibrosis?
Treating pseudomonas infections in cystic fibrosis is challenging due to the bacteria's natural resistance to many antibiotics. Over time, pseudomonas can develop additional resistance, making it even harder to eliminate. The biofilms it forms further complicate treatment, as they act as barriers that prevent antibiotics from reaching the bacteria.
How Can Pseudomonas Infections Be Prevented?
Preventing pseudomonas infections involves a combination of strategies, including regular lung function monitoring, practicing good hygiene, and avoiding exposure to environments where pseudomonas thrives, such as hot tubs or stagnant water. Vaccines and prophylactic antibiotics may also be considered for high-risk individuals.
Current Treatment Options for Cystic Fibrosis Pseudomonas
Current treatments for cystic fibrosis pseudomonas focus on managing symptoms and slowing disease progression. Antibiotics, such as inhaled tobramycin or aztreonam, are commonly used to target the bacteria. In severe cases, combination therapies or intravenous antibiotics may be necessary. Additionally, airway clearance techniques and anti-inflammatory medications play a vital role in managing the condition.
Read also:Discover The Magic Of Calypso Saratoga Springs Your Ultimate Getaway Guide
Emerging Therapies on the Horizon
Researchers are actively exploring new therapies to combat cystic fibrosis pseudomonas, including phage therapy, which uses viruses to target and destroy bacteria, and novel antibiotics designed to penetrate biofilms. Gene editing technologies like CRISPR are also being investigated for their potential to address the root causes of cystic fibrosis.
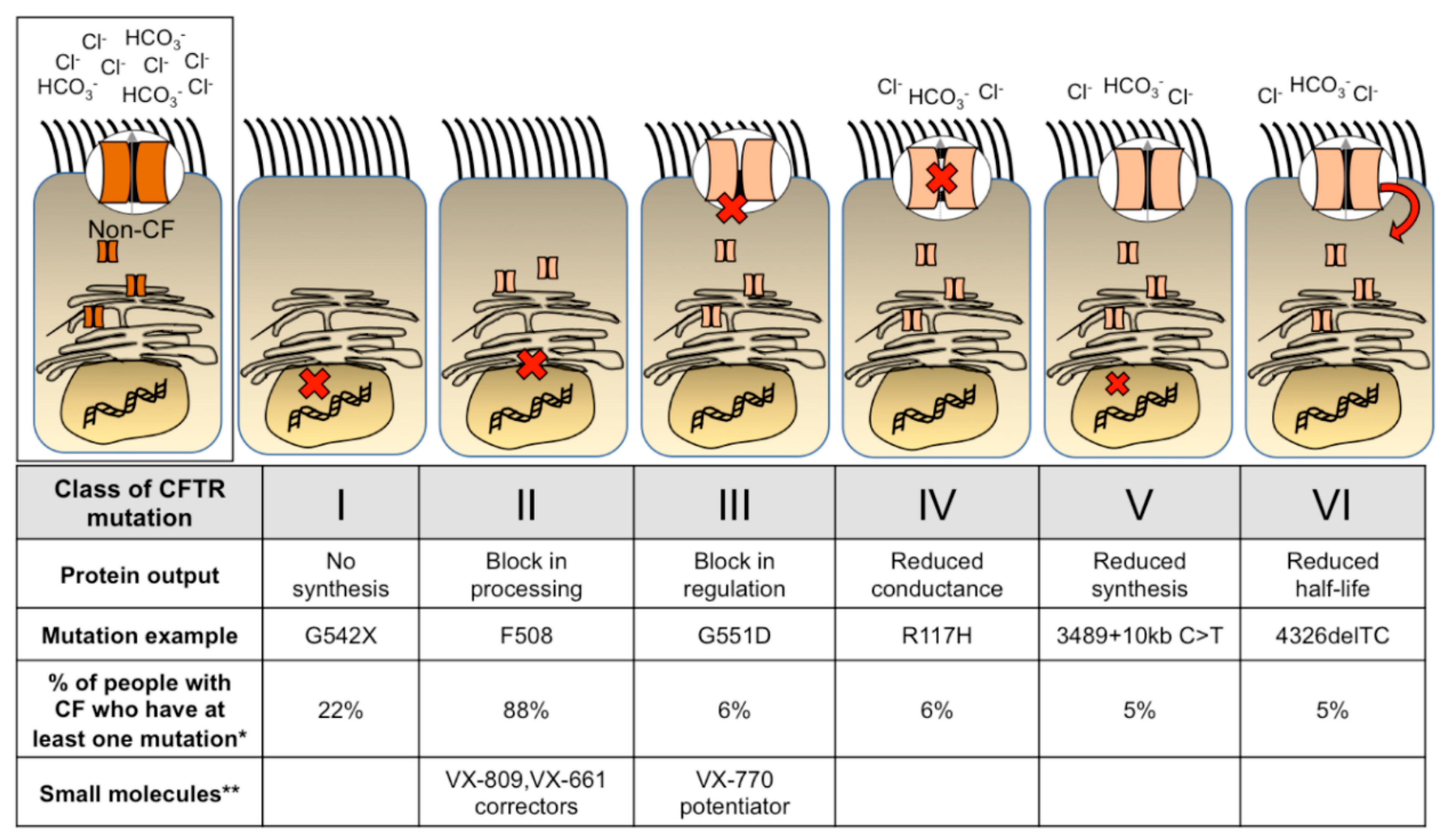
What Role Does Genetics Play in Cystic Fibrosis?
Cystic fibrosis is caused by mutations in the CFTR gene, which regulates the movement of salt and water in and out of cells. These mutations lead to the production of thick mucus, creating an ideal environment for pseudomonas to thrive. Understanding the genetic basis of the disease is essential for developing personalized treatments.
How Can Patients Manage Their Condition Effectively?
Effective management of cystic fibrosis pseudomonas requires a proactive approach. Patients should adhere to their treatment plans, attend regular check-ups, and maintain open communication with their healthcare providers. Lifestyle modifications, such as a balanced diet, regular exercise, and stress management, can also improve overall well-being.
Frequently Asked Questions About Cystic Fibrosis Pseudomonas
What is the prognosis for cystic fibrosis patients with pseudomonas infections?
The prognosis varies depending on the severity of the infection and the patient's overall health. Early detection and treatment can improve outcomes, but chronic infections may lead to a decline in lung function over time.
Can cystic fibrosis pseudomonas be cured?
While pseudomonas infections cannot be completely cured in many cases, they can be managed effectively with the right treatment plan. Advances in research offer hope for more effective therapies in the future.
How often should cystic fibrosis patients be tested for pseudomonas?
Regular testing is essential, especially for patients with a history of pseudomonas infections. Healthcare providers typically recommend sputum cultures and lung function tests at routine intervals.
What lifestyle changes can help cystic fibrosis patients avoid pseudomonas infections?
Patients should prioritize hygiene, avoid exposure to contaminated environments, and maintain a healthy lifestyle. Vaccinations and adherence to prescribed medications are also critical preventive measures.
In conclusion, cystic fibrosis pseudomonas is a complex and challenging condition that requires a comprehensive approach to management. By staying informed, working closely with healthcare providers, and embracing new advancements in treatment, patients can take control of their health and improve their quality of life. With ongoing research and innovation, there is hope for even better outcomes in the future.